Is Your Pelvic Floor a Missing Piece of Your Digestion Struggles?
We chat with Marnie, Trauma informed Pelvic Floor Physiotherapist at the Healthy Peach Physio in Brisbane Australia

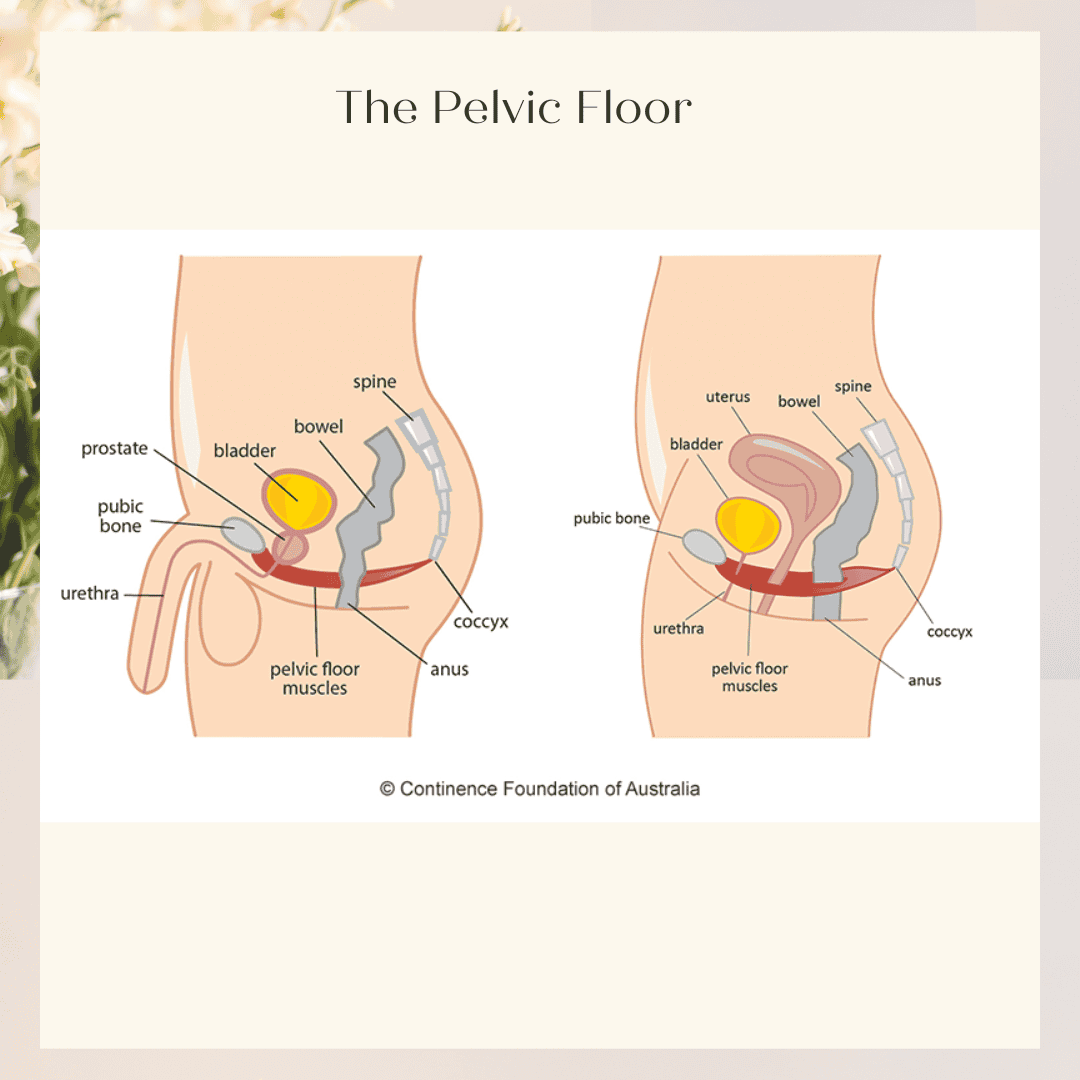
What Is the Pelvic Floor and How Does It Work?
Wait, what? Why haven’t I heard about this before?…….Where even is it exactly?
“Because you can’t see it! The Pelvic Floor Muscles line the “floor” of the pelvic bones. This fab group of muscles contract and relax without you even realising, all day! We only pay attention to them when they stop behaving in our best interest.” – Marnie Poiner, the Healthy Peach Physio, Pelvic Floor Physiotherapist
What Does the Pelvic Floor Do?
- “When it’s not a good time to go:
-
- The superficial layer of the pelvic floor muscles close the urethra (to keep urine in until we’re ready to empty), close the vagina (if you have one) and close the anus (to stop wind or stool coming out when we aren’t ready).
- When the time is right:
-
- They also open to facilitate emptying our bladder and our bowels, and to create space for vaginal or anal penetration.
- The deeper layer of the pelvic floor muscles act as a sling or hammock for the pelvic organs. They lift our perineal body (the space between the vaginal and anal opening or behind the testicles), and contract forward to the pubic bone, kinking the rectum, vagina, and urethra. You could say they’re our second line of defence keeping our bladder and bowels continent. These muscles also lengthen to create space for vaginal and anal penetration.”
-Marnie Poiner, the Healthy Peach Physio, Pelvic Floor Physiotherapist
Common Issues When the Pelvic Floor Isn’t Working Properly
Sometimes these muscles don’t behave the way we need them to, and this can lead us to having issues with:
- Holding or emptying our bladder
- Holding our bowels
- Emptying our bowels
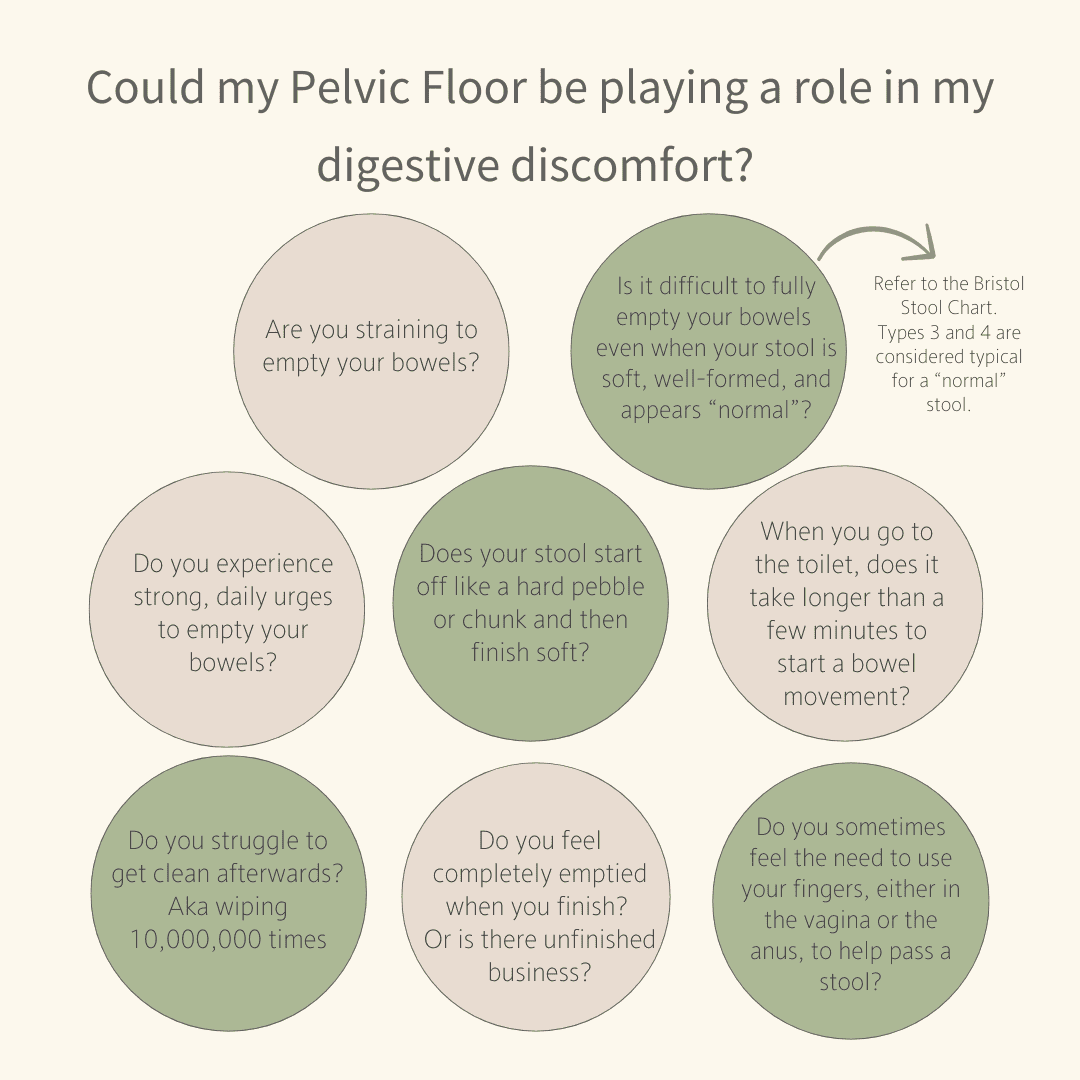
- Do you frequently get a sense of incomplete emptying?….or “not being totally finished with a bowel movement”? Struggling with bloating AND constipation?…….
- Creating enough space to have comfortable (and enjoyable) vaginal and/or anal penetration
- Ability to achieve orgasm
- Worsening of persistent pelvic pain experience
- Amplified period pain
-Marnie Poiner, the Healthy Peach Physio, Pelvic Floor Physiotherapist
How Your Pelvic Floor Affects Digestion and Bloating
Hand up if you struggle with bloating? (odds are high that if you are reading this that hand might be going up).
Bloating is consistently reported as the most distressing digestive symptom our clients are experiencing at Wander and Nourish Nutrition. So know that you aren’t alone if this is true for you.
What makes your bloated belly unhappy may be quite different from the next person so it’s important to share what is going on and seek support from trained and qualified health care providers including your GP who can help support any appropriate referrals and investigations.
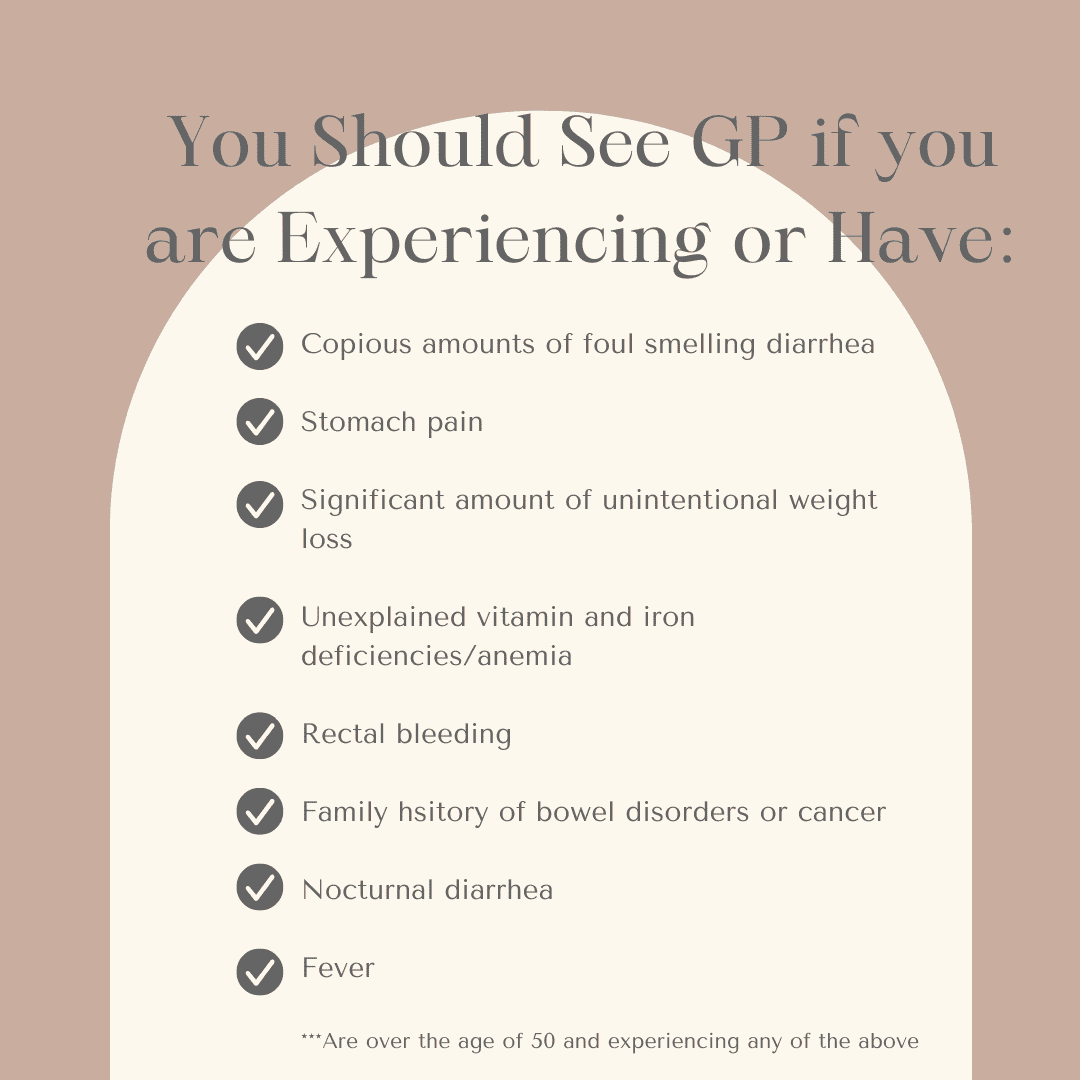
Bloating can be a symptom of many different conditions and various organs or body systems so before you start restricting/eliminating or supplementing lots of things it’s important to rule some conditions with your GP. Bloating coming from Irritable bowel syndrome for example needs different support and interventions than bloating coming from irritable bowel disease, PCOS or celiac disease.
Your pelvic floor could also have something to do with your bloating and gas struggles.
If your pelvic floor is not letting contents out easily, completely and on a regular basis (possible hypertonic pelvic floor/ overactive pelvic floor) then they are hanging out for much longer in your colon than is ideal.
One thing the colon is great at?
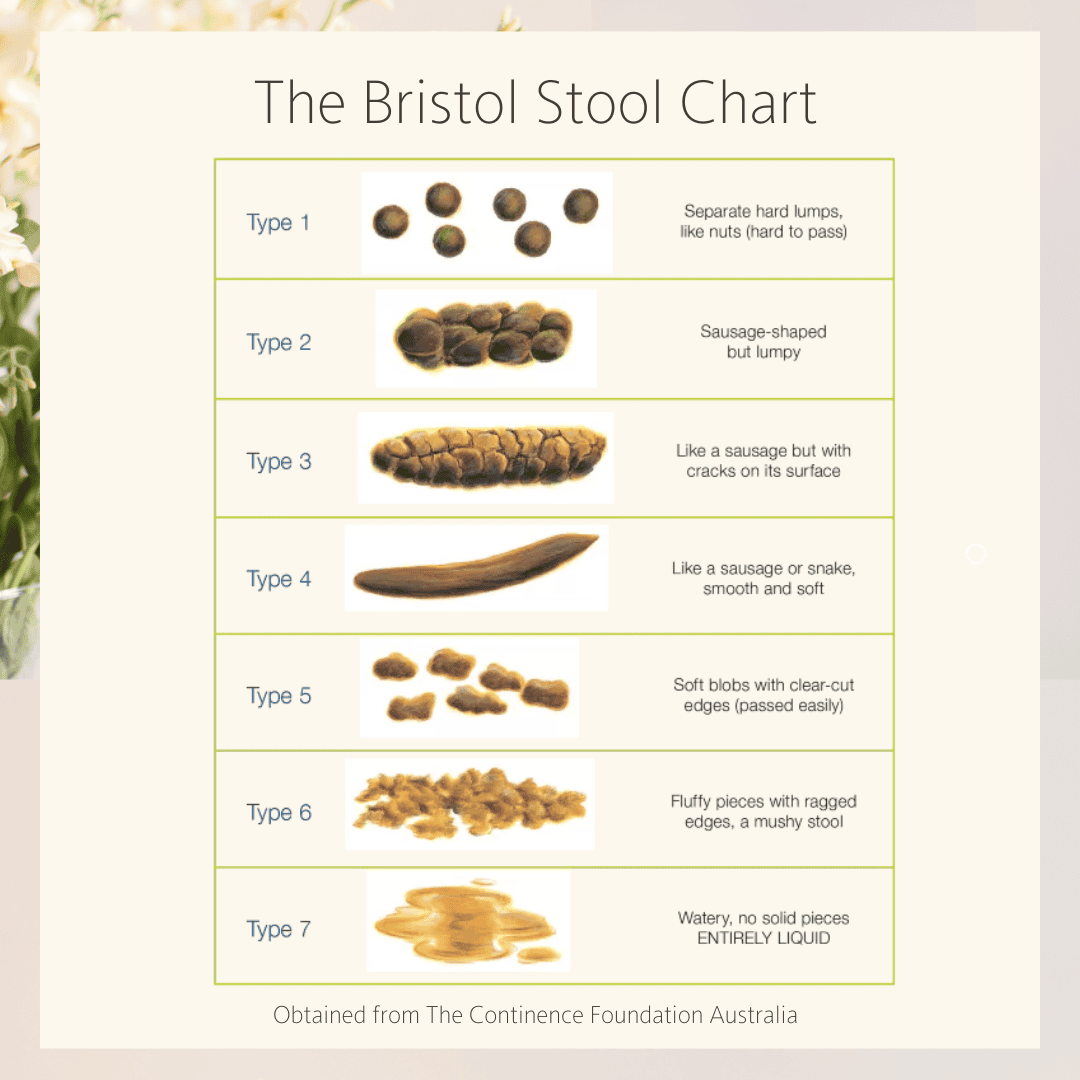
Absorbing the most fluid out of that stool it can before it exits. This means that because that stool is hanging out for longer before it leaves it is getting more and more dried out. This translates to hard to pass stool (and a lot more discomfort for you).
If this is quite bad/frequent it means other things in that digestive pipeline can get backed up (think more stool and gas trying to move through the digestive pipeline to exit and being unable to do so well or completely due to stuck stool being in the way and the exit door (hypertonic or overactive pelvic floor) not letting things out easily). U-N-C-O-M-F-O-R-T-A-B-L-E.
These challenges and sensations can worsen body image, relationship with food and eating and quality of life.
Often we find that in focusing our work together on finding what tools and supports work well for someone’s bowels to help get them moving more regularly and smoothly this helps alleviate some of the digestive challenges that are higher up in the digestive tract (for some clients this is actually all they need and they find they don’t have to restrict or eliminate foods much if at all).
As a reminder, some bloating and gas are actually signs of a healthy and well functioning digestive tract. We want to consider when these sensations feel really intense and distressing or are constant/frequent as to what else is going on or not coordinating and working as we might like.
Straining to try and move dried stool or even regular stool through an exit door that doesn’t want to open readily can also result in haemorrhoids or fissures (tears) which of course make bowel movements and bowels feel even worse.
Pelvic floor dysfunction commonly co-occurs with several digestive conditions, gynaecological symptoms and urinary symptoms as well as challenges with food and eating such as disordered eating and eating disorders. We know people living with pelvic floor dysfunction can benefit from receiving support for a Dietitian while importantly going through pelvic floor physical therapy. This is true for example if you need IBS support AND pelvic floor support.
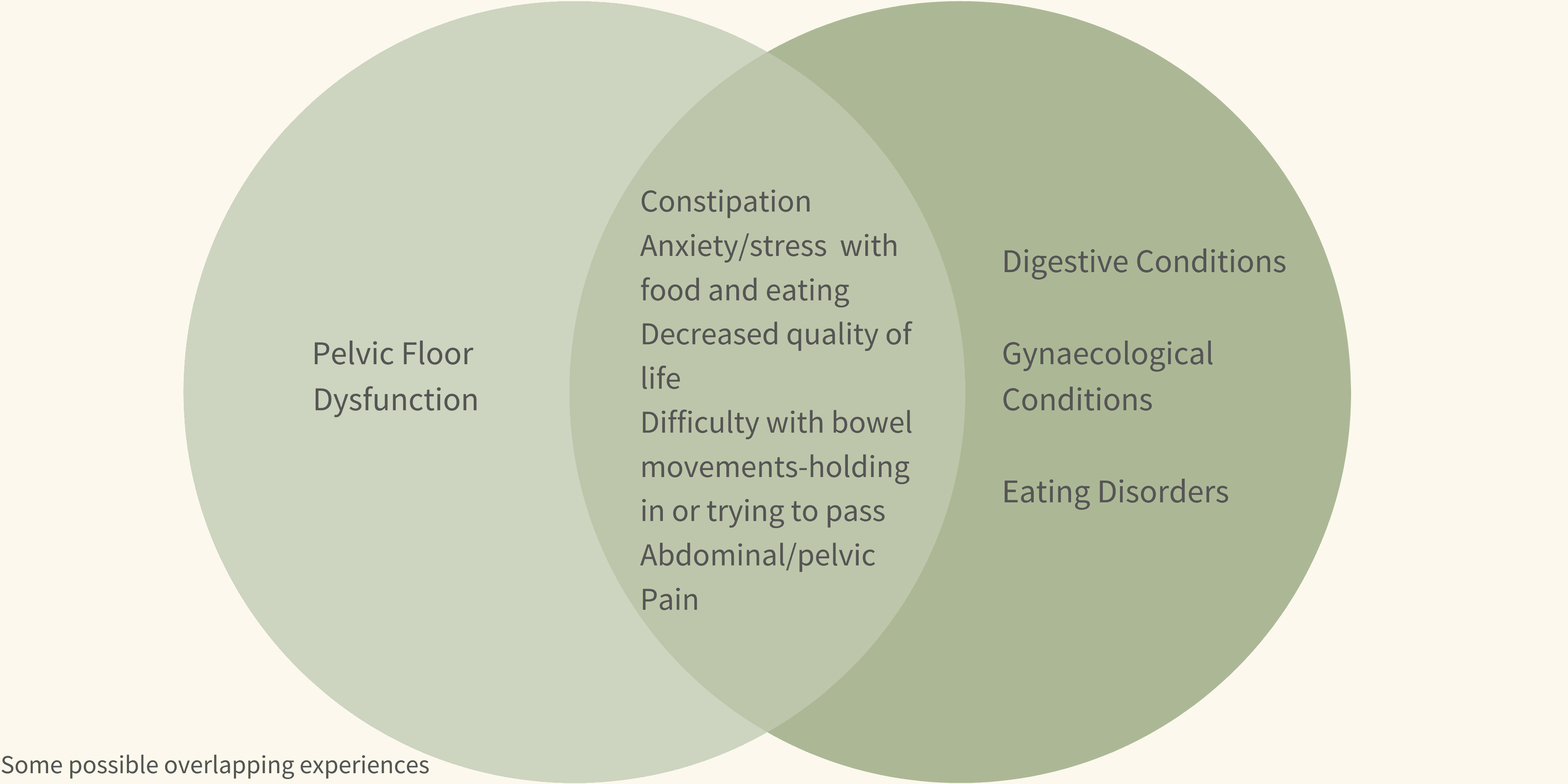
We strongly encourage that before you embark on elimination diets like the low FODMAP diet, another diet to stop bloating and gas or reaching for a smattering of different supplements to try and feel better to check in first with your GP and then likely with a Dietitian trained in digestive disorders, disordered eating (fodmap diet if wanting to explore) and possibly also a *trauma informed Pelvic Floor Physiotherapist (*not all physios are trauma informed or trained in pelvic floor care).
A trauma informed provider puts your physical and emotional safety at the pinnacle of your healthcare. They understand that your past experiences will impact how your body is behaving, and work with you in collaboration to find the most suitable treatment for you. A good healthcare provider should make you feel empowered in the treatment choices you’ve made. -Marnie Poiner, the Healthy Peach Physio, Pelvic Floor Physiotherapist
Engaging unnecessarily, or without support, in restrictive eating patterns can for many people actually ultimately worsen their digestive health and overall well being.
Restrictive eating behaviors and diets can cause new digestive symptoms, result in changes in the microbiome, changes to appetite signals and cues, increased anxiety around food and eating and cause harm to someone’s relationship with food.
We know you want to feel better!
Trust us when we say we want that for you to. We truly feel joy when clients share they have had a great poop. Truly.
How a Trauma-Informed Pelvic Floor Physio Can Help
- Mechanics of breathing
- Prescription and training on specific products/aids
- Sensitivity retraining
- Pelvic floor strengthening or down-training
- Education
- Toileting routine
- Biofeedback therapy
- Interferential therapy

The Wander & Nourish Approach to Digestive Health and Pelvic Floor Care
Our approach to your care and digestive struggles is:
- Evidenced based and informed by your lived experience
- Designed to safe guard or help heal your relationship with food and eating
- Oriented at adding things in to manage your symptoms instead of removing them (whenever possible)
- Considers and discusses with you other providers and support tools you might need to help you achieve your goals and feel better (food isn’t always the root problem or the sole solution)
- A thoughtful and gentle layered approach. We introduce dietary strategies and tools over time so you can be confident in what does work well for you vs getting lost in the weeds/overwhelmed by too many new or different things on the go at once.
- (Is it really worth taking that expensive supplement? Do I really need to avoid dairy? How much does stress or my menstrual cycle actually play a role for me?….etc).
First time checking in with your pelvic floor?
We know sometimes a little conversation starter/ ice breaker can help. Some ways to check in below.
Interested to learn more about your pelvic floor or think you might need some more tailored support for your bowels and digestion?
- Check in with your GP (you may benefit from a referral to a Gynaecologist or other provider/s)
- Come see us at Wander and Nourish Nutrition
- Contact the Healthy Peach Physio Team
Read more about pelvic floor health here